With severe internal diseases, poor nutrition, as well as with age, the growth of the nail slows down, its structure undergoes changes. Only a doctor can accurately determine the cause of the violation based on the results of tests and microscopic examinations.
But to get an idea of what happens to the nails on the legs or on the hands, you can use the photo with fungal diseases of different types.
Causes of nail deformity
Mold, yeast-like fungi, and dermatophyte fungi cause infectious nail disease (onychomycosis), which has similar symptoms.
All types of nail or hand fungus deform the nail plate, change its transparency, shine, color, this variety can be seen in the photos shown.
Changes in the nail occur not only with onychomycosis, but also with injuries, chronic paronychia (inflammation of the nail fold), psoriasis, eczema of the hands, dermatitis. Before concluding that you have a fungal infection, you should consider all of the possible options.
Signs of a fungal infection
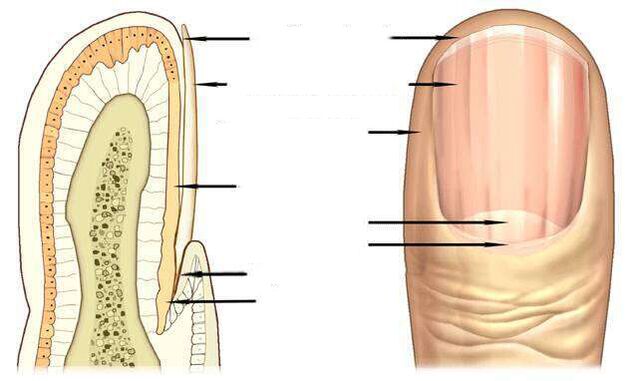
The most informative signs of fungal infection are changes in the color of the nail plate, the presence of nail detachment, superficial changes - transverse and longitudinal grooves on the plate of thenail, point depressions, thickening, destruction of the nail.

The pink color of a healthy nail is determined by the transparency of the nail plate and the blood vessels visible through it. With onychomycosis, the nail loses its transparency, the color becomes brownish, yellow, less often green, black.
The fungi and dermatophytes Candida cause onycholysis - the separation of the affected part of the nail. When infected with dermatophytes, onycholysis is observed from the far edge of the nail, and when infected with Candida, the nail lags behind the nail bed at the base, in thecrescent moon area.A symptom of a candidal fungus may be inflammation of the lateral periungual ridges - paronychia. This disease has bacterial forms caused by streptococci and staphylococci, as well as non-infectious forms - eczema, psoriasis, systemic vasculitis.
When the toenails are affected by the fungus Trichophyton rubrum, the plaque is affected, as you can see in the picture, the roller is not affected by the infection. The plaque becomes yellowish, strongly thickens, the accumulated fungal masses stand out well below.
Nail fungus due to dermatophyte infection
In 95% of all nail fungus cases, the disease is caused by the dermatophytes Trichophyton rubrum and Trichophyton mentagrophytes.
Trichophyton rubrum infection
Onychomycosis begins when the fungus penetrates under the nail plate from the free edge. Fungal infection is indicated by the appearance of a yellowish spot, an uneven, crumbling surface of the distal (distant) edge of the nail in the area of the stain.
Thedistal-lateral formof fungal infection with Trichophyton rubrum dermatophyte is common. In the photo, you can see that the spot caused by the introduction of the fungus is located along the lateral periungual crease of the nail.

The fungus Trichophyton rubrum, as a rule, affects the big toes, causing hyperkeratosis - a buildup of fungus between the nail plate and the nail bed, which looks like a loose yellowish lumpon the picture.
At this stage, the fungus occupies an insignificant part of the nail, as in the photo shown, and with the help of local treatment it is possible to cope with the incipient onychomycosis.
Without treatment, the stain grows, gradually affects the entire edge of the nail, then moves towards the half-moon. In the photo, the nail fungus looks like yellowish stripes directed to the growing area of the nail plate.
Withthe distal form of the nail fungus, which is often found on the big toes, a yellowish patch of infection appears on the distal edge of the nail, in its central part, as can be seen in the photo.

In the advanced stage of the fungus on the legs, several nails are affected, as in the photo, and the treatment is no longer limited to local remedies and pills. In addition to antifungal drugs, the nail is subjected to equipment cleaning, to remove the nail plate in whole or in part.
Long-term therapy with the use of all known antifungal agents and treatments should be carried out on the leg, caused by Trichophyton rubrum, with hyperkeritosis, as can be seen in the photo.
The fungal infection with total nail damage spreads to the whole area of the nail plate, the nail is completely destroyed.
Infection with another representative of dermatophytes, the fungus Trichophyton mentagrophytes, can also lead to total fungal infection of the nail.
Infection with Trichophyton mentagrophytes
With a total defeat of the nail with the fungi Trichophyton mentagrophytes, the nail plate is deformed, the photo shows that it thickens, changes its structure, collapses, yellowish spots appear all overits surface.
Infection of the nail with this dermatophyte usually causes superficial white onychomycosis of the big toe, less often of the little toe.
This fungus practically does not occur on the nails of the hands, it often causes interdigital dermatophytosis on the legs, as in the photo, and requires simultaneous treatment of the skin of the feet and nails.
A symptom of fungal nail infection, usually on the feet, is white spots of various sizes, like in the photo, reminiscent of leukonychia - a disease of the nail plate itself.

But unlike leukonychia, in which white spots are caused by the appearance of air bubbles in the layers of the nail, white spots in fungal infection are the result of activityof Trichophyton mentagrophytes.
Rarely, superficial white onychomycosis is caused by molds; in AIDS, the causative agent of this type of fungus can be Trichophyton rubrum and affects the fingernails and fingernails.
Toenail changes due to Candida infection
The fungus usually occurs in women, it affects the fingernails of the working hand, which is more often in contact with water.
For candidal onychomycosis, the proximal form of infection is characteristic, in which the fungus first affects the nail fold of the base of the nail, then enters the growth zone and thenail bed. Then it gradually moves along the nail from base to edge, capturing an increasingly larger area of the nail plate.
The causative agent of the disease in candidal onychomycosis is Candida albicans. This fungus invades the toenails and fingernails, extending from the half-moon area at the base of the nail plate, to the free edge, as can be seen in the photo.
A sign of Candida nail infectionalbicans is inflammation of the nail fold (paronychia), separation of the cuticle from the nail plate, pain, discharge of pus when a bacterial infection is attached.
Candida albicans is able to penetrate the nail and its free edge. In this case, they are talking about the distal form of infection, which is usually associated with skin candidiasis.

Treatment of candida fungus on the nails of the hands and feet with lesions on more than half of the area of the nail plate, as in the photo, includes not only the fight against onychomycosis, but also measures to reduce the activity of candida in the natural reservoirs of their storage - the intestines, the oral cavity, the genital mucosa. . .
Mold infestation
Molds cause fungi much less frequently than Candida or Dermatophytes. The main symptom of nail mold infection is, as you can see in the photo, thatchanges the color of the nail plate to blue, black, greenish.
Signs of nail mold can be dark spots, dots on the nail plate or, as in the photo, a black longitudinal stripe.
Preparations against fungi
Antifungal agents with fluconazole, ketoconazole, terbinafine, itraconazole, griseofulvin are used to treat nail fungus caused by dermatophytes, as in this photo.
Antifungal agents based on terbinafine are effective against dermatophyte infections.
Antifungal agents with voriconazole are very active against dermatophytes.
Itis used andto treat nail moldon the feet, hands andagainst candida yeast. The spectrum of action includes molds such as Aspergillum, Fusarium, Penicillium.
Itraconazole preparations are resistant to mold.
Fungus-like nail diseases
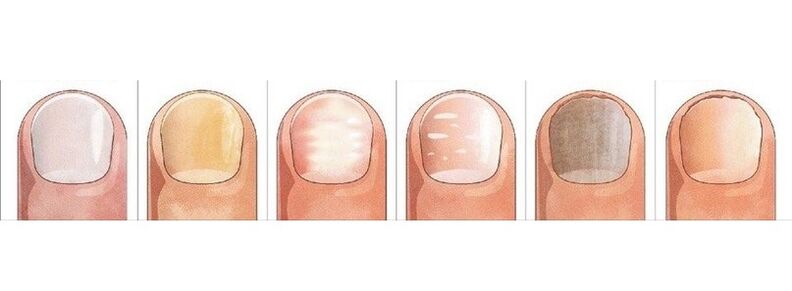
A grayish tingesometimes appears on the nailwith eczema. In this case, the nail plate can move away from the nail bed, which is observed with a fungus.
Externally very similar to onychomycosismanifestations of psoriasis. With this disease, not onlycolor changes, but alsothe nail plate thickens.
Point depressions are found on its surface, the separation of the nail plate from the nail bed is noted. But there are differences with the fungus: in psoriasis, the detached and healthy parts of the nail are separated by a pink stripe that turns yellow over time.
Thebluish colorgets the nailwith pseudomonas nail infection. Frequent mechanical friction of the nail fold causes the appearance of superficial grooves, waving of the nail.
White spots of leuconychia, the appearance of which isassociated with metabolic disorders, can also be confused with a superficial white fungus with a large area of the spot.
Changes in color, shape of the nail causing injury. The big toes are the most exposed. The nail with an injury, as well as with a fungus, thickens and darkens.

The difference between the injury and the fungus is that the changes during the injury are noted only on the injured finger, the nails of other fingers remain unchanged, do not get infected from the diseased finger, as in onychomycosis.
The consequence of trauma can be partial separation of the nail from the nail bed, the formation of a cavity, which under unfavorable conditions is quickly colonized by fungi.
The nail plate can be separated from the nail bed under the influence of light (photoonicholysis), with iron deficiency anemia, hormonal diseases. The division, loss of the nail occurs with lichen erythematosus, bullous dermatosis, trauma to the nails.
But you can finally make sure that the conclusion is correct and start treatment, you can only do this after seeking help from a dermatologist - a specialist in skin diseases, or d'a mycologist - a doctor who treats fungal diseases.





























